 see bottom of post for ingredients.. see bottom of post for ingredients.. This one is kind of a quickie. I'm going to get back to the "pregnancy interventions" series later this week, but I thought that it might be helpful to give some tips on HOW to include some "sacred foods" from these traditional cultures into your preconception or pregnancy diet. Not all of us are ready to jump into liver and onions; I know that I wasn't!! It's okay to go slow, but including at least some of these foods can only be helpful to your body and to your baby. And don't forget Dad! Cultures that prized these foods also included the father in the preconception period; he was also expected to eat liberally of whatever food was prized in fertility for his particular area. I'm going to start with homemade bone broth. Broth is incredibly nutritious and healing, and may even be palatable if you are coping with morning sickness in your pregnancy. Please keep in mind that the quality of bones is important; healthy animals will produce a more nutrient-rich, tasty broth. Buy local or pastured as much as possible, especially if you will be using the bones.
2 Comments
 Fish eggs have long been a part of the diets of traditional peoples, especially during preconception, pregnancy, and early childhood. Fish eggs have long been a part of the diets of traditional peoples, especially during preconception, pregnancy, and early childhood. A Little Back-Story I thought I'd change up the topic from purely birth-related information to something else that I feel strongly about- preconception and prenatal nutrition. I started out my first pregnancy like the majority of Americans...I absolutely believed the majority of mainstream health advice and thought that a low-fat, mostly vegetarian diet would be healthiest and help me to maintain a healthy weight and avoid cancer, heart disease, and other chronic illnesses. I exercised faithfully and consumed way too much cereal and tofu (I sincerely believed that tofu was delicious! Perhaps because it had been so long since bacon, haha). Despite my strict adherence to this dietary dogma, I found myself with a very slow metabolism and increasingly worse anxiety over really unimportant things. I tend to be a calm individual, so I felt this wasn't really "me". A doctor that I visited suggested that I had PCOS, which I didn't believe, although he assured me that "I have seen many cases of PCOS, and that's what you have. Where would you like to pick up your prescription?". Yes, he really said that, without a verified blood test or anything. I declined and a week later received an email admitting that I did not have PCOS and that I must just have "a slow metabolism". Go figure. Thanks for nothing. The tests did establish that my cholesterol was VERY low. The doctor thought this was good, but I wasn't so sure. SURPRISE! 3 weeks later I find out that I really stink at Fertility Awareness Method (I had been using it for a whopping 5 months) and I'm pregnant! Another nail in the coffin for PCOS. I very fortunately had no morning sickness and spent the first 12 weeks of the pregnancy in denial, but when I saw the tiny baby on the ultrasound screen at that first 12 week appointment, I knew....I NEED TO LEARN ABOUT BABIES. I had never planned on having children. I never even babysat. My daughter was the first newborn that I had ever held. I was woefully unprepared. I jumped into researching and discovered cloth diapers, elimination communication, normal birth, and everything else I could find. I also noticed that I started craving foods that I didn't usually eat. Butter. Eggs. Bacon. Whole milk. I had lived most of my lives using these foods very sparingly, but I couldn't deny that I now needed those foods. And when I started allowing myself those foods during pregnancy...I became happier than I had been in a long time. Turns out there is a good reason for that. Nutrient-Dense Food Makes You Happy and Healthy My body was craving eggs and butter because my low-fat diet had deprived me of a lot of nutrients that need FAT to be properly utilized by the body. The depletion of these nutrients was likely contributing to my anxiety, because your body needs fat and cholesterol to regulate hormones and mood. Building a baby requires a LOT of nutrients. My body knew that I needed to beef up on natural vitamins A, D, and K. Most people know that if the mother is deficient in certain nutrients, the body will steal these from the mother's body to preserve the baby as much as possible. But many women now have been on low-fat, processed food diets for ten years or more! A woman who is having a baby at 25 may have been dieting (as I had been) since she was a teenager. Many women are now waiting until after their careers are established to start a family, and may have been dieting for 15+ years before conception of a child. This absolutely can affect the health of the mother during pregnancy, AND the baby's development. Dr. Chris Masterjohn summarized some of the common denominators in prenatal and preconception diets of traditional cultures studied by the dentist and researcher Weston A. Price. (Interestingly enough, Weston Price expected to find that healthy groups isolated cultures would be eating mainly vegetarian or even vegan diets. Instead, he found that the groups with the healthiest reproduction, resistance to disease, and minimal cavities consumed diets balanced in vegetables, properly prepared grains, and nutrient-dense animal products). Here is an excerpt of a very detailed article that you can read in it's entirety here. "All groups that had access to the sea used fish eggs; milk-drinking groups used high-quality dairy from the season when grass was green and rapidly growing. Some groups used other foods such as moose thyroids or spider crabs, and African groups whose water was low in iodine used the ashes of certain plant foods to supply this element.5 These foods were added against the backdrop of a diet rich in liver and other organ meats, bones and skin, fats, seafood and the local plant foods." Did you get that? Fish Eggs Whole Raw milk from grass-fed dairy (including butter and cheese) Thyroid glands Shellfish Organ meats Bone broth Local plant foods and grains Sounds crazy, right?? Gross, even? Why were these foods so important? Weston Price stated that all of these peoples would go to great lengths to obtain these foods for their pregnant and nursing mothers. They couldn't run to Trader Joe's or Whole Foods. Sometimes they would travel for days to procure fish and shellfish. Turns out that these foods contain large amounts of vitamins D, A, K, and other nutrients such as calcium, phosphorus, sulfur, iodine, and zinc. All of these are necessary for optimal development of the baby's brain, skeleton, reproductive system, eyes...everything! Liver and other organ meats are a great source of Folate, which is known to prevent many varieties of birth defects. Although some studies have shown that too much folic acid can contribute to some cancers, folate is the natural form of this nutrient and is essential for developing babies, and there is no known harmful limit. Vitamin A deficiency has been shown in numerous studies to contribute to birth defects, and plants contain a form that is not utilized effectively by many individuals. Preformed vitamin A is found abundantly in organ meats, shellfish, fish eggs, and raw, grass-fed dairy. The advantage to using whole foods, no matter how foreign to us personally, over prenatal vitamins, is that foods generally contain a balance of essential nutrients, as opposed to a high concentration of one or the other. Take fish eggs, for example. Dr. Masterjohn explains: "Fish eggs are especially rich in cholesterol, vitamin B12, choline, selenium, calcium, magnesium, and omega-3 fatty acids. They contain a modest amount of most fat-soluble vitamins but their vitamin K2 content is unknown." All of those nutrients are available from one tablespoon of fish eggs! If you're not a fish egg person, try a free-range, local chicken egg, which provides most of the same nutrients. I have grown to love egg yolks and I'll add them to pretty much anything for an instant, natural multi-vitamin boost. Now I know why I craved eggs during my pregnancy! I'm glad that I gave into those cravings for whole milk and eggs, because despite my previous low-fat diet I did have a healthy baby, and my moods stabilized. I am never looking back, and guess what? My addition of butter, ghee, whole raw milk, and plenty of eggs to my diet have not packed on the pounds. I'm basically the same size I was before, but about 10 pounds lighter. The joke was on me. Whole foods keep you healthy, and your baby healthy! (Also, they taste really good!)
There is WAY too much to write on this topic; this article doesn't even scratch the surface. If you want to learn more about foods and nutrients that can help you during your pregnancy and for optimal development of your baby, stay posted for future blog posts or give me a call. I can talk about this stuff ALL DAY. I also recommend reading Dr. Masterjohn's entire article, Vitamins for Prenatal Development, Conception to Birth. You may also be interested in this book, Beautiful Babies.  I initially started by wording this question, "What routine interventions should I opt out of at the hospital," then I realized that this question is really about a lot more than what just goes on once you get to the hospital. So, I'm going to point out a few interventions that are likely more harmful than helpful
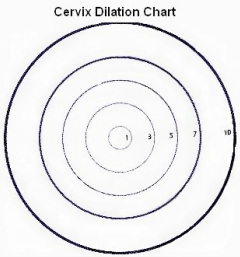
What You Can Opt Out of During Pregnancy Cervical exams, including membrane sweeps. At your prenatal appointments towards the end of your pregnancy it is expected that when you get into the exam room, you will take your clothes off and the doctor does a pelvic exam to check the length and dilation of the cervix. WHY? If you are not having contractions, this is largely a useless, but also potentially harmful practice. Randomized controlled studies show that it's not even helpful to predict or prevent preterm labor, much less to predict when normal labor will begin or not. The cervix is NOT a magic 8 ball! It cannot tell you, or anyone else, when you will go into labor. Let me repeat this, because even most doctors and nurses may not tell you this. THE CERVIX IS NOT A MAGIC 8 BALL. Why is this important to remember? Imagine this: A woman goes in at 37 weeks and the doctor finds that her cervix is dilated to 2cm and starting to thin out. The doctor says, "Congratulations! You're going to have a baby within a week!" But a week goes by...and another....and she's still pregnant. When he offers an induction at 39 or 40 weeks the chances are high that she will take it, because, after all, she should have had her baby already! Maybe her body can't even go into labor?! What would you do if this were you? Remember that the end of pregnancy is a very vulnerable time, and it's easy to get discouraged by the suggestion that your body is not "preparing" for labor. The opposite scenario can be just as damaging. What if a woman went to all of her last few appointments and cervical checks revealed that she was not dilated at all as she neared her due date. She might start to feel like "nothing is happening", "my body can't do this on it's own." Again, if the care provider brings up induction for any reason, she may accept out of resignation, thinking that her body just isn't progressing fast enough. This is simply NOT TRUE. A woman could be not dilated at all at her appointment, but have a baby that night, or walk around at 4cm, 5cm, or MORE for weeks! I have personally talked to women who experienced all of these scenarios, so please don't worry about what your cervix is or isn't doing! Or, as the OB told me during my first pregnancy. "Just keep your pant on when you come in if you don't want cervical checks". Good advice. Membrane stripping/ "sweeping" is commonly done during cervical checks to "get things moving". The membranes that make up the amniotic sac are literally teased away from the cervix. However it's worded, this is an intervention that is done to start labor. This is known as INDUCTION. It may or may not work, and there is conflicting evidence of it's safety, but it is absolutely an intervention that you do not have to consent to unless you choose to. Here is a midwife's perspective on this common practice, and why you might want to think seriously before accepting this intervention. This study found that 70% of women found the procedure to be very uncomfortable, and 30% described it as "significantly painful". Labor started, on average, one day sooner with the group that received the membrane stripping. My own personal observation is that membrane stripping can be uncomfortable (even painful), and if labor does not start, the mother can experience painful contractions that rob her of comfort and sleep in an otherwise already uncomfortable time in her pregnancy. If labor does begin, she may be very tired and worn out psychologically, and if it doesn't, she has been put through such discomfort for nothing. Membrane stripping may be something to consider if the mother is being threatened with a more medical induction, since it certainly has less risks than cytotec or pitocin.
Multiple ultrasounds, especially as you near your due date I've already written one blog post about this, but just to review a few of the reasons why late-term ultrasounds are almost completely unhelpful and might even cause false alarm. There are no studies that show that ultrasound in a low-risk pregnancy can accurately predict size of the baby, state of the placenta, or health of the baby, including amniotic fluid levels. Yet these are the measurements that are frequently used towards the end of pregnancy to justify induction of labor. I can't possibly go into all of these excuses for induction in this blog post, but I can provide links. Here is a great evaluation of the lack of evidence for induction due to low fluid in a term pregnancy. Here is why induction for a "big baby" is also not supported by ACOG OR evidence. Ask yourself, "What am I hoping to see on ultrasound, and what will I do with that information?" "What will my doctor want to do with that information?" The basic fact is that unless there is indication of another problem (bleeding, preterm labor, reduced fetal movement, etc), ultrasound provides generally unreliable information, and is not without risks. I'll have to leave the next set of interventions for my next blog post! I should have known that this would be super long. Next week- What You Can Opt Out of During Labor
What You Can Opt Out of After the Birth
If you're not from Charlottesville, this might seem like a really strange question! But, if you have lived here for any length of time, you'll likely understand why I'm writing on this topic. In this area we are privileged to have two good hospitals. They both have their advantages and disadvantages, and BOTH are becoming more and more "natural birth" friendly. University of Virginia hospital, for example, is now delaying clamping the umbilical cord at all births, even cesarean births! Although evidence-based and safe, this practice has been slow to be adopted in many hospitals, so I am SO happy that even mothers and babies who require cesareans will be able to benefit from delayed cord clamping if they are at UVa Hospital.
Martha Jefferson Hospital has the reputation of being more natural-birth-friendly, and they have the advantage of a brand new (as of last year) hospital and birthing wing, set to beautiful scenery above Charlottesville. No kidding, I was recently told by a husband that they considered a home birth, but went to Martha Jefferson Hospital for the view! You can see a picture of the labor tubs here. This hospital does have a relatively low epidural rate (around 60%), so I can understand why it has the reputation of being THE place to go for a natural birth, but does that mean that a doula wouldn't be helpful, or just a waste of your resources? NOT AT ALL. Here's why. Choosing a doula lowers your risk of surgical birth. Your chances of cesarean are still much higher at a hospital than at home or a birth center, no matter the hospital. In 2010 the cesarean rate at MJH was 34.2%, compared to 30.7% at UVa hospital, despite the higher rate of unmedicated births at MJH hospital. See the numbers for yourself here. UVa also had double the percentages of VBAC births of MJH. (The local birth center here, The Birth Centre of Charlottesville, has a 3% cesarean rate as of last year). Randomized trials found that the use of a doula reduced a mother's chance of c-section by 28%! There are a few hypotheses as to why doulas are so effective, and you can read more about them here. Nurses have lots of other things to do, they cannot fill the role of a doula. They also change shifts. While there are many great nurses out there that wish they could be as supportive as a doula, they are limited by the rules, policies, and other duties that they must perform as a nurse. Some of these include charting, taking blood pressure, checking in on other patients, putting orders into the system, and communicating with other staff and doctors. Even in a hospital like MJH where there is a "one-to-one" nurse to patient ratio, this is typically guaranteed only during "active" labor. Continuous labor support is one of the most important factors in an empowering and healthy birth experience, and nurses cannot be continually with their patients, even if they wanted to be. They also are limited by the clock. You may have a nurse that you really "click" with, and who loves to help couples who desire a low-intervention, natural birth, but when the shift changes, the next nurse may not be so comfortable with your plans. I've certainly read stories of nurses staying past their shift to help out a special couple...but the reality is that nurses are not paid to be on-call! You doula is, though, and she will be with you for the entire labor and birth if at all possible. Your doctor's policies and practices are even more important than the hospital that you choose, especially at a private hospital. A public hospital like UVa can enact hospital-wide policies (like delayed cord clamping) and it's likely that all doctors, residents, and nurses will implement this. At a private hospital your care can vary more depending on the practices of the individual physician. If you choose this physician, for instance, your chance of a c-section would be 33%! However if you chose this physician, your chance would be lower, at 21%. (The Virginia Department of Health seems to not have updated this data since 2008, so this data may not be representative of these providers' current rates, but my point about variability stands.) Other policies may vary, also. One doctor may allow intermittent monitoring for a VBAC (vaginal birth after cesarean), but another might want continuous monitoring. One may enforce a strict 12-hour time limit on labor after membranes have ruptured, and another might be more comfortable waiting longer. Some obstetricians may be quicker to induce for "post-date" pregnancy than others. These interventions increase the risks of instrumental birth, fetal distress, and cesarean section no matter which hospital you are at! A doula bridges the gap and evens the playing field by providing support and evidence-based information so that mom and dad can decide which interventions they are comfortable with at the time. I do believe that you can have an empowering, healthy birth experience in the hospital. But, a hospital is a hospital no matter how pretty it looks on the outside (or inside). Having a doula ensures a certain continuity of care- you know that your doula is supportive of your plans, will not change shifts, and can help you to navigate hospital or provider policies. Together, you can have a great birth, no matter where it takes place! |
Author- Sara
I look at birth from the perspective that our bodies are wonderfully made, and if we really believe that and work with the birth process and nourish our bodies properly, they will function optimally, most of the time! Archives
November 2019
Categories
All
|

 RSS Feed
RSS Feed
